How Do You Get People Into Addiction Treatment if They Don’t Want It?

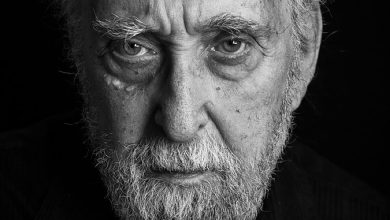
Fifteen years ago, I was the father of a child who was living on the street, addicted to meth, opioids and other drugs. My son was slowly dying.
When he was missing, I scoured neighborhoods where I knew he hung out. Mostly I searched in vain, but I found him a few times and tried to persuade him to enter a treatment program. He was unwilling to get help. He became angry and belligerent. He accused me of trying to control him. He insisted he was fine and said he could stop using on his own if he wanted to, but he didn’t want to. Once he was 18, I couldn’t force him. He had to decide for himself — and yet he was in no condition to do so. “I was completely out of my mind, unable to make rational decisions,” he says now.
Most people who are seriously ill want to get better and, if given the opportunity, will choose to be treated. However, addiction can defy logic.
“You can only understand what it’s like to be addicted if you imagine being deprived of air,” a boy addicted to opioids once told me when I visited an adolescent treatment program for book research. “You’ll do anything in order to breathe. You’ll kick, punch, knock down walls. I didn’t want drugs; I needed them — that’s how it felt — and I did whatever it took to get them. I lied, cheated and stole. I would do anything for drugs.”
This is why substance use disorders, if untreated, can lead to criminal behavior, debilitation and — all too often — death. The number of overdose deaths in the United States is higher than ever.
Ideally, people with addiction would seek care. But waiting for a person to choose treatment for a disease that affects rational thought can be catastrophic, now more than ever. The ubiquity and lethality of street drugs such as fentanyl and fentanyl mixed with xylazine, a veterinary tranquilizer, mean that many people with substance use disorders are in grave and imminent danger, and most cannot simply quit on their own.
This is excruciating for people with loved ones addicted to drugs. I spent years in abject terror waiting for the phone to ring in the middle of the night, afraid of being told, “Mr. Sheff, we have your son. He didn’t make it.”
In November 2022, when Mayor Eric Adams of New York announced that the city would begin sending people with untreated mental illnesses to hospitals, even against their will, the controversial decision resonated with me. He said the city had a “moral obligation” to help them. I believe that moral obligation extends to people with substance use disorders. I would have wanted someone to intervene with my child on the street using potentially lethal drugs and admit him to a hospital. As unpopular as that decision may be, I would have supported it even if I knew my son had been taken into care against his will.
There’s a common view that people with addiction can’t be helped unless they choose to go into treatment. But the data on voluntary versus coerced and court-mandated treatment is not so clear-cut. Some studies show people don’t need to choose treatment for it to be effective, even though it may be more effective if they choose it willingly.
“The fashionable rhetoric is that mandating people doesn’t work, but evidence points the other way,” says Keith Humphreys, a professor of psychiatry at Stanford University and an expert in addiction medicine.
One study he cites, published in The Journal of Substance Abuse Treatment in 2005, followed patients one and five years after voluntary and court-mandated treatment. It concluded that “contrary to popular belief,” when drug users mandated to treatment are compared with people who sought treatment themselves, those who were mandated had similar results related to drug use outcomes and reductions in crime “or sometimes better than those achieved by voluntary patients.” The study also indicated that recognizing they have a problem and being motivated to stop using “may not be necessary for salutary changes to occur, either in the short or longer term.”
Not every expert agrees, and there are also studies questioning the long-term efficacy of compulsory treatment and the risk of potential harms, especially in programs that fall short of standard of care. The data can be difficult to parse because there are many different levels of coercion and ways that people can be pushed into treatment programs — and different treatment protocols when they get there.
The National Institute on Drug Abuse says the evidence for compulsory treatment is mixed. “Creating a climate that encourages and supports people to seek treatment voluntarily and provides access to evidence-based treatment methods is critical,” the group said in a statement. “When that fails to happen, systems and organizations may begin to look to coerced treatment as an alternative.”
To understand whether compulsory treatment works, the institute says, “one must first ask if that treatment is evidence-based and also consider both short-term outcomes like halting drug use and long-term outcomes like staying in recovery.”
I understand why involuntary and coerced treatment are viewed negatively. The approach is part of what brought us the disastrous and counterproductive war on drugs. But with the current state of the drug supply, those who love people with substance use disorders have a difficult choice: Do something, even if it’s deeply unpleasant and may not ultimately work, or risk their loved one’s death.
There are effective ways to get people into treatment who don’t want it. One of the most effective intervention methods is community reinforcement and family training, or CRAFT. Unlike many interventions depicted on television, this approach to encouraging people to get treatment isn’t characterized by blame, threats and ultimatums but by expressions of love, empathy and support. Data suggests that about two-thirds of interventions using CRAFT succeed in getting people into treatment, but it isn’t an option for many people with acute manifestations of addiction, especially for those who are alienated from their families, unemployed or isolated.
When an approach like CRAFT isn’t possible, we need other methods to intervene and encourage people to seek treatment. Health workers should try by reaching out to people wherever they are — on the streets, in encampments for the unhoused, at food banks and at medical clinics where individuals with addiction sometimes go. Mr. Adams recently announced a plan to send more counselors and medical professionals into the streets of New York City.
Another opportunity to intervene is at emergency rooms, syringe exchanges and safe-consumption sites, where they exist. Most are underground. Sites like these are greatly underfunded and technically illegal. We need more of them. Last year, 700 overdoses were reversed at New York’s OnPoint overdose prevention centers, and trained staff members were able to get some people to enter treatment.
There’s also coercion, which worked for my son. He used dangerous drugs for 10 years before he went into a program that finally helped him. He didn’t want to go, but he broke into his mother’s house and was about to be arrested. A sympathetic police officer gave him a choice between rehab or jail. He chose rehab. If he hadn’t been impelled, he says (and I believe), he probably wouldn’t be alive today. There was a time I didn’t think he would make it to 21. He turned 40 this year, after being sober for 11 years.
But not all involuntary treatment needs to be, or should be, mandated by the criminal justice system. We don’t want to wait for people to fall into the criminal justice system before they are helped. People have also been forced to choose between treatment and, for example, being kicked out of the house, being left by a partner or losing a job. In some cases, this type of coercion works, though it can also backfire. If an attempt fails, a person can become even more alienated and recalcitrant.
One of the major problems with involuntary treatment is the poor quality of many programs. Many people forced into treatment are not given evidence-backed care. They are left to painfully detox without access to medications that can make the process easier and likely more effective. They are often not treated with respect. Many are threatened, blamed and badgered. And if a person’s experience is negative, it could mean they are less likely to try treatment in the future.
Whether they are in an outpatient or a residential program and regardless of how they got there, people with substance use disorders must be cared for by professionals trained in addiction medicine. They must be offered therapies such as cognitive behavioral therapy and contingency management and medications like buprenorphine that prevent overdose and cravings for opioids. Programs should also assess and treat patients for co-occurring psychiatric disorders; at least 40 percent of those with substance use disorders have one or more. This would be a major improvement for most programs, potentially changing the outcomes.
Many people in the traditional recovery world believe that we must wait for people who are addicted to hit bottom, with the hope that they’ll choose to enter treatment. It’s an archaic and dangerous theory. Many people die before they hit bottom. We must intervene, and interventions followed by evidence-based treatment can reverse the downward spiral that often accompanies dangerous drug use. If an intervention doesn’t work the first time, we must try again. And again. Because where there’s life, there’s hope.
David Sheff is the author of “Beautiful Boy: A Father’s Journey Through His Son’s Addiction.” He founded the Beautiful Boy Fund to make quality, evidence-based care available to people suffering from problems related to drug use and addiction and identify and support research to further the field of addiction medicine.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips. And here’s our email: [email protected].
Follow The New York Times Opinion section on Facebook, Twitter (@NYTopinion) and Instagram.